Image Gallery
Frequently Asked Questions about Fibroid Embolisation
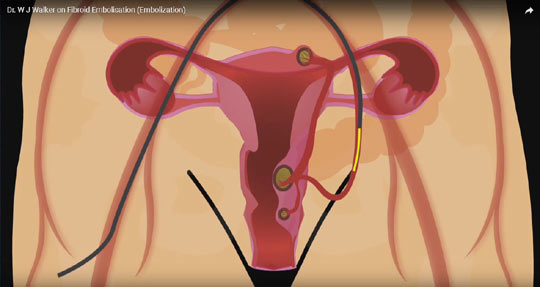
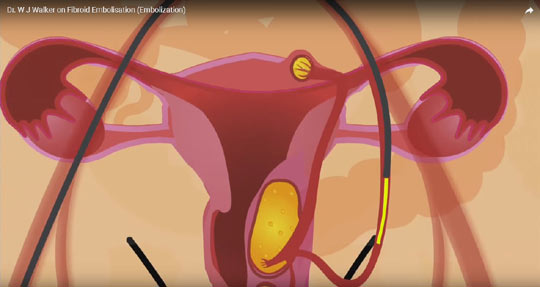
What happens to the particles that are injected into the uterine arteries?
The particles are made from PVA (poly vinyl alcohol). They are reduced to the size of under 1000 microns and look like little grains of sand. These particles are completely inert and have been used in embolisation procedures for many decades. They cannot cause any harm and gradually disintegrate over a period of time.
Can the particles be placed in the wrong artery?
Yes it would be possible to inject particles into the wrong artery instead of the uterine artery: particles could be injected into other branch vessels, eg which supply the bladder and rectum, and such complications have very rarely been recorded. This is why it is important that the doctor doing the embolisation is an Interventional Radiologist who is particularly experienced in fibroid embolisation so that this complication would not occur. In our series we have had no complication of this nature in over 2,400 cases.
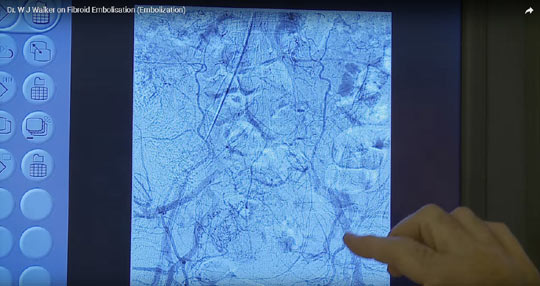
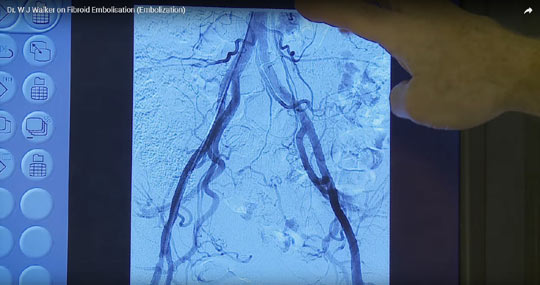
Can the procedure fail from a technical point of view?
Yes this is possible because the uterine vessels may come off the main trunk at a very difficult angle that makes it difficult to catheterise with the tiny catheter that we use for these procedures. The rate of technical failure is related to operator experience. It can be as high as 10% or higher when inexperienced operators perform the procedure. In our case the technical failure rate is minute and well below 1 in 100; in which case a second attempt is usually successful.
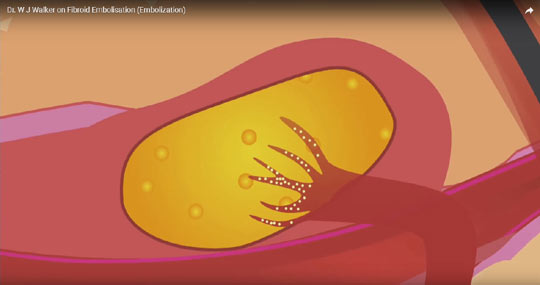
Can the procedure fail to kill all the fibroids?
Yes it can, but again this relates to technical expertise. In one series they recorded a failure to kill the dominant fibroid of 30% (Mara et al 2008). This problem again is due to operator inexperience. It is rare in our series that the fibroids are not all infarcted, in particular the main or dominant fibroids. The usual reason for failure to kill all the fibroids is that insufficient particles are instilled into the uterine artery.
What is the recurrence rate after fibroid embolisation?
The answer to this question is that the recurrence rate is very low. Often so-called recurrence is due to the fact that all the fibroids have not been killed and one or two small ones have then grown. The recurrence or regrowth is again rare when the procedure is carried out properly and probably of the order of around 2-3% and is more likely to occur in Afro-Caribbean women. If recurrence does occur this can be simply rectified with a repeat embolisation.
How bad is the pain following an embolisation procedure?
Nobody knows exactly what the precise cause of the pain from fibroid embolisation is. It is to do with the dead fibroids and in our experience there appears to be more pain when the fibroids have more blood vessels in them. Overall, subjectively about one third of our patients get mild pain, a third get moderate pain and a third get pain that would be considered severe. However, with the right cocktail of drugs the pain is controlled. Its duration is variable tending to be maximum in the few hours after the embolisation procedure. By 12 hours the pain is usually a mild dull pain and the patient is eating and drinking normally. In our protocol patients are got up 4 hours after the embolisation procedure and are ambulant. When the patients return home they may get some attacks of pain and are supplied with pain killers.

What other symptoms can I expect after fibroid embolisation?
After an embolisation procedure, most patients suffer a mild degree of what we call post-embolisation syndrome. It is characterised by a rather washed out feeling, there may or may not be a mild temperature for 2-3 days and the abdomen can feel rather bloated. This all subsides within the first week to 10 days. By week 3 most of our patients are back at work.
Can I get pregnant after fibroid embolisation?
The answer is yes: in our series we have had 75 successful completed pregnancies after uterine artery embolisation. The main alternative to embolisation is myomectomy ie surgical excision of one or more fibroids. Either procedure may be appropriate and the decision may be complex. The question of fertility following fibroid embolisation and questions revolving around the procedure in patients desiring fertility is explained in much more depth in our internet site fibroids.co.uk within the Fertility Section and anyone who has fibroids and is thinking of either surgery or embolisation should read that section.

I have a condition called adenomyosis – can this be cured by embolisation?
Adenomyosis is a not uncommon condition where cells from the lining of the womb migrate into the muscle of the womb and cause heavy periods and bleeding. It is not a malignant or cancerous condition. The normal treatment for this condition is hysterectomy. The condition however can be cured with an embolisation in approximately 50% of cases. In the remaining 50% the symptoms of adenomyosis may recur and probably around half of those can be cured by a second embolisation. In patients with adenomyosis, unless it is extremely florid, embolisation is a good option and has very high patient satisfaction rates on data analysis. Again patients should read the section headed Adenomyosis on our internet site.
How long should I take off work after a fibroid embolisation?
The normal period is two weeks as general advice. However, it depends on a number of factors. If the fibroids are small probably the patient may do light work after one week; if the fibroids are large e.g. over 20 weeks pregnancy size then two weeks may be appropriate but we normally advise three if the patient has a relatively arduous job.
What causes fibroids?
There is no simple answer and a great deal of research is currently being carried out on this subject. There is certainly a significant genetic element and if you have fibroids it is likely that other relatives in your family will also have fibroids. Fibroids are sensitive to hormones - oestrogen, progesterone and growth hormones - but particularly to oestrogen and fibroids contain increased numbers of oestrogen receptors. However, one should always bear in mind looking at the incidence and genesis of fibroids, that 30-40% of women have fibroids and, of course, in many of these women the fibroids do not cause any significant problems.

Do alternative cures for fibroids work?
The answer is no. If these cures worked for fibroids it would be extremely simple to perform a series where you carried out MRI scans on say 20 patients and showed that following the alternative medicine therapy the fibroids shrunk. Suffice it to say, that no such series has been carried out and in my experience of scanning many patients who have tried alternative therapy, it has made absolutely no difference to the size of the fibroids.

Is drug treatment for fibroids of any value?
The answer is that in some cases drug treatment such as Norethisterone, a progesterone like hormone GNRH antagonist which modifies the release of certain pituitary hormones and puts you into a temporary menopause, and a drug called Esmya, may be appropriate in certain cases where bleeding is heavy. The problem is drugs such as GNRH antagonists and Esmya can only be used for short periods of time and may cause quite significant side effects. Following withdrawal of these drugs any improvement in the fibroids is negated and symptoms rapidly return. In the case of Norethisterone again this may be only partially successful in controlling periods and may have significant side effects. In many cases a more definitive treatment eg surgery or uterine artery embolisation will be the better option. Where bleeding is not due to fibroids affecting the lining of the womb, other procedures such as transcervical resection of the endometrium, Mirena coil insertion (a progesterone secreting coil) may well solve the problem.
What sort of anaesthetic is administered?
Patients are sedated with drugs injected into a vein. Most patients are asleep for most of the procedure.
Will I be in hospital for the embolisation?
Yes, following the embolisation procedure we monitor people in hospital for one or two nights ensuring that their pain is controlled properly. Where embolisations are carried out properly and all the fibroids are killed, if patients are discharged prematurely, they may need readmission for pain control. It is therefore our policy to stabilise patients in hospital.
Is fibroid embolisation a new procedure?
Emphatically no, the first embolisation procedure was carried out in 1986 by a French neuroradiologist. It is accepted and recommended by NICE in the UK and by the Colleges of Obstetrics and Gynaecology and Radiology in the UK and in the USA. For further details see our website.

What about fertility?
This is a complex question but in our series we have had 74 women who have had successful completed pregnancies after embolisation. The decision in patients wishing to conceive as to whether you should have fibroid embolisation or surgery, i.e. myomectomy can be complex in some cases. The pros and cons of surgery and myomectomy with regard to fertility patients are discussed in the Fertility section of our website and patients who are in that situation are strongly urged to read that section carefully before making a decision.
When can I try to get pregnant after fibroid embolisation?
Our advice is to wait approximately five months after the embolisation when the uterus will have ‘settled down’ although patients have conceived successfully before this.
Will my sex life suffer after fibroid embolisation?
Mid and long term follow up of patients after fibroid embolisation has not shown any adverse affect on a patient’s sex life after the procedure.

What happens to fibroids after they are killed?
They shrink down and are converted by the uterus into small balls of scar tissue. They are harmless. The procedure is curative on long term follow up in over 95% of cases.

References
Mara M, Maskova J, Fucikova Z, Kuzel D, Belsan T, Sosna O. Midterm clinical and first reproductive results of a randomized controlled trial comparing uterine fibroid embolization and myomectomy. Cardiovasc Intervent Radiol 2008;31:73-85
© Copyright 2015 • All Rights Reserved | Dr. W.J. Walker |